Unquestionably, the healthcare industry is changing. The demands of contemporary, digital, value-based care models are causing traditional reactive systems to disintegrate. Patients want better, quicker, and easier access to treatment. Regulatory agencies, however, want quantifiable advancements and reliable, real-time data. Healthcare platforms must actively promote improved results; digitizing current workflows is no longer sufficient.
At the core of this change is the incorporation of Digital Health Quality into platform designs. Healthcare platforms demonstrate how AI-powered, intention-focused, modular systems may revolutionize the industry. This thorough investigation combines important ideas to provide a concise, empirically supported, step-by-step knowledge of how advanced platform design and digital health quality standards are revolutionizing healthcare.
Increasing Need for High-Quality Digital Health
Beyond Conventional Clinical Results
The definition of healthcare quality has expanded significantly during the past ten years. It presently consists of:
- Timeliness: Quick reaction to the demands of the patient.
- Accessibility: Fair access for all demographic groups.
- Cost-Effectiveness: Utilizing fewer resources while optimizing care.
- Integrity of Data: Reliable, up-to-date health information.
The effectiveness with which digital technologies can improve patient, clinical, and operational outcomes, rather than merely transferring paper workflows onto screens, is what defines the quality of digital health.
Key Principle:
The influence of technology on performance, not simply its presence, is what true digital health quality evaluates.
Digital Infrastructure Development: From Antiquated Systems to Contemporary Platforms
Limitations of Legacy EHRs
Older systems:
- Data silos between departments
- Delay information that is essential to patient care
- Oppose interoperability initiatives
These disparities obstruct coordinated care and ongoing quality enhancement.
The Development of Digital Platforms That Are Modular
Modern digital health platforms employ designs that are modular and decomposable to:
- Integrate payers, care teams, and EHR data sources.
- Integrate clinical reasoning and AI into routine tasks.
- Encourage in-the-moment decision-making through ongoing quality assessment
- Quickly adjust to regional laws and medical practices
Examples from the Real World: Frameworks such as the WHO-ITU Digital Health Platform Handbook and initiatives like India’s ABDM support modular digital health ecosystems.
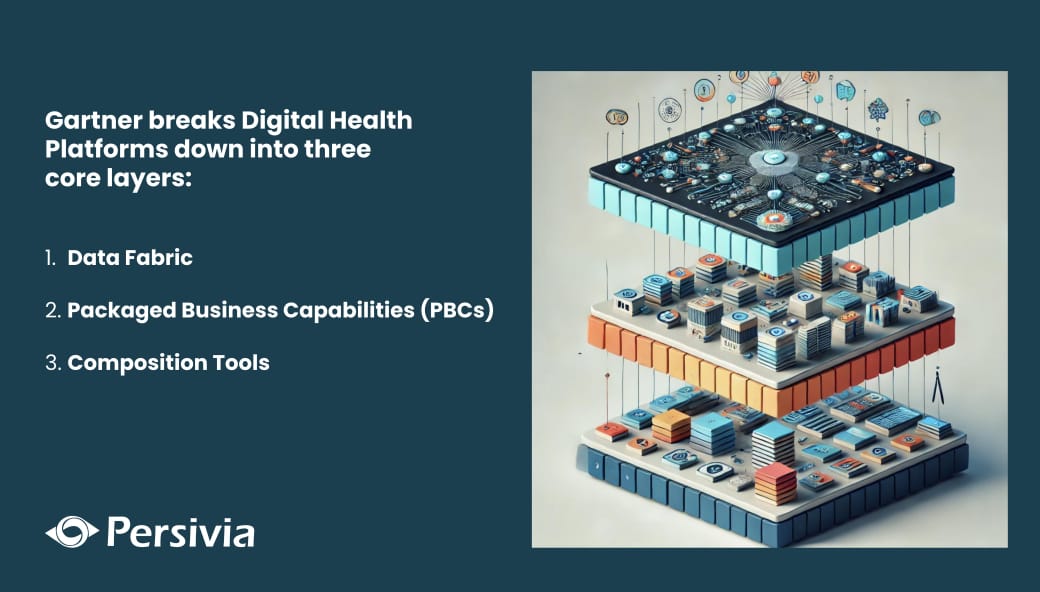
Composable Platforms: The Foundation of Superior Digital Health
Composability: What Is It?
Packaged Business Capabilities (PBCs) are modular components that make up a Composable Platform. Every PBC carries out a distinct healthcare-related task, such as care coordination, digital engagement, or risk management.
Benefits of Composable Architecture:
- Reuse Parts: Quicker innovation without system rebuilds
- Quick Deployment: Faster fixes for new problems
- Regular Data Governance: Workflow-wide uniform policies and controls
Data Governance and Accuracy: Creating Reliable Health Data
The Significance of Governance
Effective governance guarantees:
- Actionable, trustworthy data
- Reduced inconsistencies and duplication
- Strong clinical significance for every piece of information
Crucial Elements:
- Active Metadata Mapping: Tracking ancestry and data changes
- Clinical Background: Making sure it is not simply a technical convenience but also a medicinal relevance
- Instantaneous Visibility: Dashboards and notifications for real-time patient tracking and judgment
Note: In the absence of robust governance, data turns from an asset to a burden.
Features of High-End Digital Health Platforms
Top-performing platforms are superior because they offer:
- Scalable AI-Native Systems: Designed to expand and change to meet healthcare demands
- Real-Time Care Management Tools: Providing clinicians with empowerment at the moment of care
- Low-Code and No-Code Settings: Increasing personalization without IT snags
- Support for Payer-Driven Metrics: Calculating eCQMs, HEDIS, and STARS measurements with ease
Bottom Line
Digital health quality is becoming essential as healthcare prices increase, workforces get smaller, and payment mechanisms change. It is essential for strategic reasons. By proving that quantifiable clinical, operational, and financial benefits are not only feasible but also anticipated, cutting-edge systems (such as Persivia CareSpace®) are establishing the new benchmark.
Health systems of the future will be those that embrace:
- AI-first, modular, and decomposable platforms
- Robust data governance
- Operations that are goal-oriented and purpose-driven
Modernization is no longer the key to healthcare transformation; rather, it is about how well you integrate digital health quality into your systems’ core architecture.
Persivia CareSpace®: An Effective Framework for High-Quality Digital Health
The best digital health platform is Persivia CareSpace®, which has:
- Modular Architecture: Every feature is an independent PBC that is simple to update and repurpose.
- Unified Data Fabric: Integrating complete lineage control with both structured and unstructured data.
- Large-Scale Clinical AI: Insights powered by AI at each stage of the patient journey, from admission to release.
- Intention-Driven Processes: The platform coordinates the required procedures while users specify targets (such as lowering readmission rates).
With features for care management, risk adjustment, quality analytics, etc., CareSpace® serves more than 12,000 doctors and more than 200 hospitals. Explore further details now!